Health Impacts of Fuel-based Lighting
Evan Mills
Lawrence Berkeley National Laboratory, University of California, 94720 USA
Lumina Project Technical Report #10
October 16, 2012
Download Full Report [PDF] | literature review here
Working Paper for presentation at the 3rd International Off-Grid Lighting Conference
November 13-15, 2012, Dakar, Senegal
Executive Summary
The challenges of sustainability often intertwine with those of public health, revealing opportunities in both arenas for disenfranchised populations. A fifth of the world’s population earns on the order of $1 per day and lacks access to grid electricity. They pay a far higher proportion of their income for illumination than those in wealthy countries, obtaining light with fuel-based sources, primarily kerosene lanterns. The same population experiences adverse health and safety risks from these same lighting fuels.
Beyond the well-known benefits of reducing lighting energy use, costs, and pollution (which has its own health consequences), off-grid electric light can yield substantial health and safety benefits and save lives. While knowledge of these benefits can enhance the business case for conversion to more efficient and less dangerous technologies such as LED lighting, proponents often lack accurate information. Statements confusing lighting with the more widely known health impacts of cooking are a particularly common problem.
A large but specialized medical literature identifies an array of risks associated with fuel-based lighting, including: burns caused by a wide variety of factors, indoor air pollution, non-intentional ingestion of kerosene fuel by children, suppressed visual health, and compromised health services and outcomes in facilities lit with fuel-based light. Each risk factor results in illness, and most in mortalities. Lighting is the dominant and sometimes only use of kerosene (referred to as paraffin in some parts of the world) in rural areas, although kerosene plays a large role for cooking in urban areas or areas without solid fuel supplies. Lighting-only statistics are provided in this report whenever possible.
There are few national-level assessments of health impacts associated with off-grid lighting. A survey of 3,315 users of kerosene lighting across five sub-Saharan Africa countries found 26% to have health concerns related to the kerosene lighting. Many sudies report that accidental ingestion of kerosene is the primary case of child poisoning in the developing world. In South Africa alone, over 200,000 people are injured or lose property each year due to kerosene-related fires, in addition to 79,750 very young children unintentionally ingesting kerosene (in 3.6% of all households), of which 60% develop a chemically induced pneumonia. In Bangladesh, kerosene lamps are responsible for 23% of infant burns. Three multi-year reviews of admissions to Nigerian hospitals attributed ~30% of all burn cases to kerosene. Even higher burn rates (~40%) are attributed to kerosene lamps in Sri Lankan homes, with 150-200 lives lost and an associated cost of $1M each year to for medical care.
Most studies are based on hospital admissions, which vastly underestimate incident rates in the broader population, particularly among the poorest segments and other groups less likely to have access to or seek hospital care. This report’s review of 85 published reports spanning 27 countries indicates the pervasiveness of impacts and potential solutions:
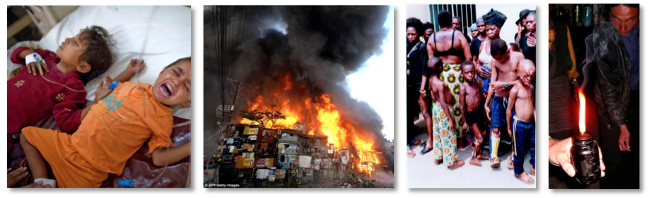
- Fuel-based lighting is a significant cause of structural fires and severe burn injuries, with particularly high death rates (24% on average) in cases where kerosene is adulterated with other fuels, resulting in explosions.
- For context, more than 95% of deaths worldwide from fire and burns occur in the developing world, and the mortality rate is 5-times higher in low- and middle-income populations in Africa than in high-income countries in Europe.
- Lamp and candle incidents cause structural fires, which can spread in tightly crowded slums, with a single event burning hundreds to thousands of homes.
- Deliberate and non-intentional adulteration of kerosene with other more volatile fuels has caused many reported explosions in kerosene lanterns and stoves, resulting in hospitalized patients with burns over large percentages of their bodies and mortality in many cases. There is a 24% average mortality rate for the studies of hospital admissions attributed to kerosene explosions. In the worst documented event, 2,500 people were injured.
- Mortality rates (all ages, excluding kerosene-adulteration explosion cases) for hospital studies averages 3%. Children are disproportionately affected.
- One long-term study found that lantern-related burns cause nearly 10% of injury-related mortalities among children in southern India.
- Indoor pollutants from fuel-based lamps include multiple hazardous materials, with concentrations of particularly unhealthful particles an order of magnitude higher than health guidelines. Correlations with cataract and tuberculosis have been observed, but require further study.
- Individuals using simple wick lamps in indoor environments will likely be exposed to dangerous PM2.5 particle concentrations that are an order of magnitude greater than World Health Organization ambient health guidelines. Less-polluting hurricane and pressure lamps may not exceed guidelines, but cause pollutant levels about 5-times greater than outdoor ambient conditions.
- Kerosene combustion products appear to be correlated with higher incidences of tuberculosis and cataract conditions, but the causal links with lighting fuels are not confirmed. In the only study to examine the lighting dimensions of the risk, researchers found the odds of having TB in Nepal were more than nine times greater for women using kerosene than those using electric light.
- Females and children spend a larger proportion of their time indoors and thus experience a greater exposure to pollutants than males.
- The available literature focuses on emissions from kerosene, with little attention to unique emissions from other fuels when used for lighting, or hazards from wicks made with lead cores or lantern mantles made with radioactive thorium.
- Unintentional ingestion of kerosene is a risk unique to children, and is typically the primary cause of child poisoning in developing countries, with an average mortality rate of 7% for the studies reviewed.
- Kerosene ingestion is the primary cause of child poisoning reported in most hospital studies. The consequences are severe, including mortality rates ranging from 0% to 25% for those visiting hospitals in the larger studies reviewed.
- A form of pneumonia (chemical pneumonitis) occurs in 12% to 40% of the cases. Central nervous system impairments also result.
- Poor illumination levels from fuel-based lanterns are only 1% to 10% of those recommended by lighting authorities in industrialized countries. Users complain of vision-related problems and irritation, but the impacts are not well quantified.
- Multiple studies find complaints about insufficient lighting and eyestrain from users of fuel-based lighting (particularly high-output pressurized lanterns), and an increased incidence of visual health problems (including near-sightedness).
- Inadequate lighting in clinics poses barriers to the delivery of quality healthcare, discourages patients from seeking care, and compounds the risks of adverse outcomes such as as maternal and infant mortality as well as infections due to the difficulty of maintaining sanitation in low-light conditions.
The nature of certain types of injuries and the demographics of exposures indicate that women and children tend to disproportionately experience the impacts. Vulnerable populations are not presented with effective or affordable alternatives. Safety information is necessary, but does not substitute for addressing the underlying role of poverty and lack of access to modern energy sources. Replacing fuel-based lighting with efficient and cost-effective off-grid electric systems provides health benefits while supporting poverty alleviation.
Replacing intrinsically dangerous fuel-based technologies is the only way to reliably eliminate the myriad risks. Grid electrification has sought to do this for many decades, but progress has been very slow. Indeed, the number of people using fuels for lighting is still increasing in some parts of the world, particularly sub-Saharan Africa. A more promising avenue for energy access are the innovative small-scale solar or grid-charged LED lighting systems, many of which provide more, better, cheaper, and safer illumination.
Available evidence indicates health-related consequences can be greatly reduced when fuel use is displaced with electric lighting. Limited surveys have documented almost complete elimination of injuries and vision-related complaints among people switching from fuel-based to off-grid electric lighting systems. Health workers and patients in clinics report improved morale and outcomes (e.g., fewer infections, more accurate blood-banking, and more successful child deliveries) when better lighting is introduced.
Policies and programs targeting the most vulnerable geographical and demographic user groups will obtain the greatest benefits. Examples include improved illumination in healthcare facilities, substitutes for fuel-based lighting where housing is dense and poorly defended from fire (slums), and where fuel adulteration is particularly common due to fuel subsidy imbalances and other factors. Improved technologies for women and children will yield the greatest benefits.
Acknowledgment. This work was supported by the Assistant Secretary for Policy and International Affairs of the U.S. Department of Energy under Contract No. DE-AC02-05CH11231. Useful data and comments were provided by Peter Alstone, Kate Bliss, Kevin Gauna, Arne Jacobson, Dustin Poppendieck, David Schwebel, Laura Stachel, Dehran Swart, and Shane Thatcher.
